A few years ago, there were many places where it would be illegal to walk into a bank wearing a mask. Today, it is illegal in many places to walk into a bank without wearing a mask. Now, I do not want to beat a dead horse. The mask argument has been proven to be ridiculous on many fronts and the arguments for masks generally center on pseudo-scientific hypothesis like viruses are transmitted by droplets. But with my country tripling down on mask use, and the fact that I have yet to write a mask article, I figured its better late than never to address the issue.
I will let the U.S. Center for Disease Control, one of the main purveyors of mask use, hit me with their best shot and analyze their literature review on masks. Of course, calling it a literature review is a stretch. They do not actually present an accurate accounting of the literature, instead choosing to omit hundreds of articles and decades of research that show masks do not work. Instead, they cherry pick bits of information from hilariously bad “studies” to make their point. In total, the CDC points to 19 studies as evidence that masks work; thus, I will be breaking this analysis up into two or three parts for readability.
USS Theodore Roosevelt post-hoc survey
CDC Claim: Masking reduced risk of infection by 70% (unadjusted OR 0.30, 95% CI = 0.17–0.52)
What the study actually says:
Prevalence of previous or current infection was higher among participants who reported contact with someone known to have COVID-19 (64.2%), compared with those who did not (41.7%) (OR = 2.5; 95% CI = 1.1–5.8); prevalence was also higher among persons who reported sharing the same sleeping berth with a crewmember who had positive test results (65.6%), compared with those who did not (36.4%) (OR = 3.3; 95% CI = 1.8–6.1). Lower odds of infection were independently associated with self-report of wearing a face covering (55.8% versus 80.8%; OR = 0.3; 95% CI = 0.2–0.5), avoiding common areas (53.8% versus 67.5%; OR = 0.6; 95% CI = 0.4–0.9), and observing social distancing (54.7% versus 70.0%; OR = 0.5; 95% CI = 0.3–0.8), compared with service members who did not report these behaviors.
My analysis:
First off, the CDC purposefully changed the language from the study to make the point more poignant; however, the true problem is they left all of the confounding factors out of their claim. Anyone that has had an introductory statistics or social science class has probably encountered the birds and the bees discussion on why correlation is not causation. Generally, this discussion will point to the useful and humorous example of shark attacks and ice cream sales.
The story goes like this: The summer resort town Amity has been seeing an increase in shark attacks lately. Concerned, they hire a young, but naive, statistician from the local college to investigate. In his quest to investigate the root cause of the attacks, the statistician begins to gather data on the town. He quickly notices that as ice cream sales increase, so does the frequency of shark attacks. The correlation, in fact, is nearly perfect! Thus, he concludes, that ice cream sales increase shark attacks.
The statistician’s conclusion is obviously absurd. There is obviously a third factor involved — namely, ice cream sales increase on hot days, and so, too, does the frequency at which people go swimming. Amity would have been better off hiring a marine biologist and a professional shark hunter than a statistician relying on correlational factors.
Looking at the results from the study, it would be safe to conclude that crew-members that were in close contact with infected individuals were much more likely to get the virus. All of the other factors, in fact, could be roughly generalized as social interactions. So we might even conclude that those more likely to wear masks are less likely to engage with others socially.
CDC Claim: Masking reduced risk of secondary infection by 79% (adjusted OR 0.21, 95% CI = 0.06–0.79)
What the study actually says:
Families without transmission / families with transmission:
Median age 42 v. 52
Comorbidites: 13.3 v. 24.4
> 2 days hospital visitation: 57.8 v. 70.7
> 3 days laboratory confirmation: 84.3 v. 90.7
Self-awareness of being infected: 42.2 v. 24.4
> 2 days to medical isolation: 68.7 v. 85.4
Self isolation: 69.9 v. 51.2
Separate silverware: 69.9 v. 56.1
Better hand hygiene: 93.2 v. 87.5
> 3 family size: 49.4 v. 62.5
< 20 residential area per capita: 37.1 v. 50
> 4x close contact: 8.7 v. 30
< 1 bedroom per person: 65.4 v. 72.5
> 2 days room before cleaning: 27.2 v. 40
> 1 time per day cleaning with bleach: 38.3 v. 10
> 1 hour ventilating room: 76.5 v. 57.5
My analysis:
There are so many confounding factors here that this survey tells us absolutely nothing about face masks.
CDC Claim: No COVID-19 infections among 67 patrons who were tested in follow-up.
My analysis:
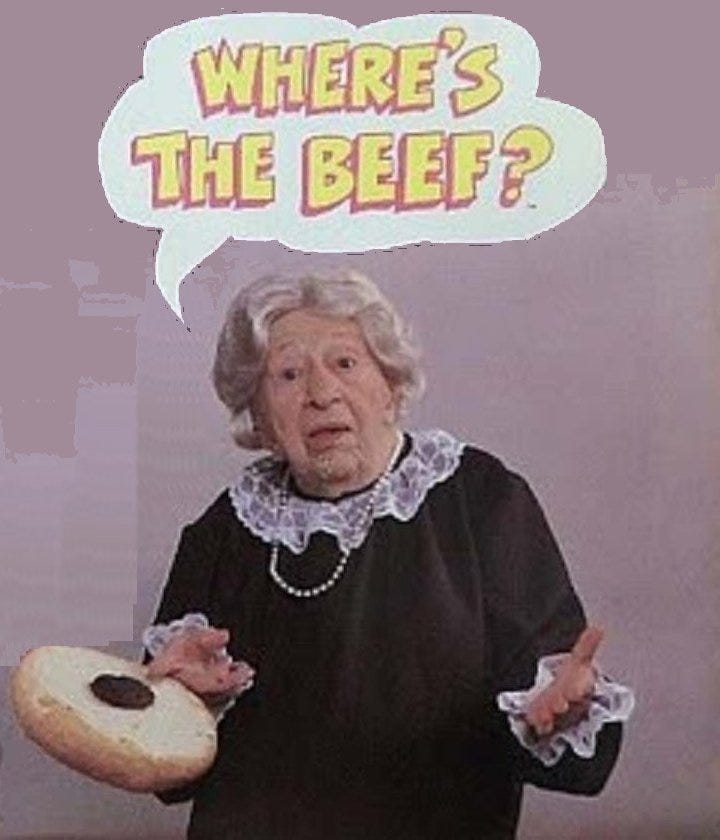
This is a weird, non-peer reviewed “paper” that only seems to appear on the CDC website. Almost everything about this paper is strange including the layout and analysis. In any case, it is a small sample size, half the patrons did not respond to the survey, the appointments were short and many of them took place long after the hair stylists would have been infectious, and usually hair stylists would be facing away from a person when cutting their hair. Nothing is controlled for and the only people that would have been interacting face to face, masks on or not, were the stylists that were both infected. Also, considering the stylists worked for a long period of time before self-isolating, one has to question how sick they were in the first place. There is also the fact that respondents could have been asymptomatic or had few symptoms worthy of testing for and may not have even known they had the virus. I don’t know what else to say besides this is not strong evidence for masks and the fact that it is continually cited as a case study for masks shows us how weak the evidence for masks truly is (is that the best you got CDC?).
Thailand Retrospective Case-Control Study
CDC Claim: Always having used a mask reduced infection by 77% (adjusted OR 0.23, 95% CI = 0.096–0.60)
What the study actually says:
This seems to be a theme, but the infected cohort was markedly different from the uninfected cohort. Infected / Control group:
Male: 69.2 v. 51.8
Infected in boxing stadium: 59.2 v. 2.3
40 years older or older: 52.6 v. 41.4
Physical contact: 67 v. 36.1
>60 minute duration of contact: 90.4 v. 60.8
Sharing dishes: 40.5 v. 31.2
Sharing cigarettes: 6.2 v. 1.4
Handwashing (often): 24.8 v. 45
Not only that but the infected group were MORE LIKELY TO WEAR A MASK at some point. The uninfected never wore a mask 60.7% of the time compared to 48.6% of the time for the infected group.
My analysis:
This is another garbage study with too many confounding factors to actually tell us anything about mask transmission. Even worse, the CDC only selected one part of the study to make a broad conclusion despite the fact that those always wearing a mask were incredibly different from those that sometimes or never wore a mask.
The Arizona trends after mandate implementation study
CDC Claim: Temporal association between institution of masking policy and subsequent decline in new diagnoses
What the study actually says:
My analysis:
The cross-sectional mask-wearing and control in the USA study
CDC Claim: 10% increase in mask wearing tripled the likelihood of stopping community transmission (adjusted OR 3.53, 95% CI = 2.03-6.43)
My analysis:
This is an example of yet another anonymous internet survey. This time they used SurveyMonkey and a Boston’s Children Hospital program to collect names that are not representative at all of the US population. They had arbitrary weighting values of mask wearing, which may or may not have had an effect on the results, but was arbitrary none-the-less (see below: why would they average the score here? Theoretically, one would be less likely to hang out with friends who they knew to be sick, but being in a grocery store is an unknown)
But really, the entire premise that a SurveyMonkey survery can tell us anything about mask wearing in the community is ridiculous. A significant percentage of respondents did not even bother to fill out the majority of the questions. The authors of the “study” admit this could be biased by social desirability bias, but really, I think that’s the least of the studies problems.
Mask use is neither observed nor estimated. Other factors like hand-washing and social interaction are not observed nor estimated. They didn’t even compare R0 with mask mandates (where people would be largely forced to wear masks), and instead noted that mask mandates do not change mask use significantly. Is that true? Then why is it that when mask mandates end, most people stop wearing masks? Maybe this is a sign that your survey is non-random? (as if being a SurveyMonkey survey was not enough of a hint at that).








Ty the Fisch feels the same way :-) https://www.youtube.com/watch?v=YzSgXonr0X0&t=29s
Fantastic analysis! If the best evidence has 100s of confounders, we should be very very skeptical. I remember asking one of the co-authors of a HCQ pre exposure prophylaxis studies in India whether considered adherence to protocol as a confounder? They said, they did and that's why they continued to push that masks must be worn for HCQ to work.
I suggested that we can't know that, because we don't know if people's adherence to PPE or their adherence to HCQ or their tolerance for SARS-COV-2 was driving the results (since people were lost to follow up, died etc.).
Anyway, it's just impossible to push these results as conclusive for anything and the way to actually test these things will never be funded.